Retinal Department


Alcon, the American company, is one of the most important and most accurate ophthalmology device companies. The INFINITY device is one of the devices used in cataract operations without surgical intervention.






What is Diabetic Retinopathy?
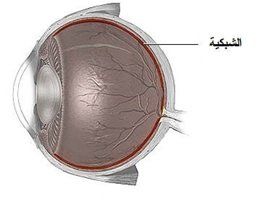
Approximately half of all diabetics will develop diabetic retinopathy. Patients with diabetes mellitus (DM) can have abnormal blood sugar levels which can damage normal blood circulation throughout the body, including the eye.
In diabetic retinopathy (DR), high blood sugar levels cause damage to blood vessels in the retina which can impact vision.
There are three main ways that diabetic retinopathy causes vision loss:
- Diabetic macular edema (DME) — fluid build-up in the central portion of the retina
- Proliferative diabetic retinopathy (PDR) — growth of abnormal blood vessels into and on top of the retina
- Iscchemia — retinal cell death or dysfunction due to lack of oxygen in the retinal tissue
Diabetic retinopathy can affect type I (insulin dependent) and type II (non-insulin dependent) diabetics. The board-certified retina specialists at Retina Consultants of Texas are trained to diagnose diabetic retinopathy and help patients manage the condition.
Types and Stages of Diabetic Retinopathy
There are two main types of diabetic retinopathy: non-proliferative and proliferative.
Non-proliferative Diabetic Retinopathy (NPDR): Non-proliferative diabetic retinopathy (NPDR) and background diabetic retinopathy (BDR) describe early stages of diabetic retinopathy. Blood vessel damage in diabetic retinopathy can lead to abnormal leakage of fluid and blood into the retina. This leakage can cause the retina to swell. If this swelling occurs in the macula, it is called diabetic macular edema (DME), and vision can be affected. This is the most common cause of visual loss in patients with diabetes and ranges from mild to severe.
Proliferative Diabetic Retinopathy (PDR): PDR occurs when abnormal blood vessels grow into and on top of the retina. These abnormal blood vessels are fragile and can bleed into the eye causing vitreous hemorrhage. This can cause dark floaters and may cause immediate and severe loss of vision. Pulling and contraction of these abnormal vessels and their associated scar tissue on the retina can lead to a tractional retinal detachment, a condition where the retina is pulled away from the back of the eye leading to loss of vision.
Causes and Symptoms of Diabetic Retinopathy
In its earliest stages, diabetic retinopathy typically has no symptoms. That is why it is important for patients with diabetes to take a preventive approach. All diabetics should see their ophthalmologist for a comprehensive dilated fundus eye exam at least once a year. In addition, it is important to control blood sugar, blood pressure and cholesterol levels. Early detection of diabetic retinopathy allows the best chance for maintaining good vision.
As diabetic retinopathy progresses, common symptoms patients may experience include:
- Blurry or distorted vision
- A decrease in visual acuity (sharpness)
- Floaters
- Muted color detection
- Vision loss
Diagnosis
Diabetic retinopathy is diagnosed by your ophthalmologist during a dilated eye exam. Your doctor may obtain photographs of the retina and diagnostic tests, including ocular coherence tomography(OCT) and fluorescein angiography (FA), to help guide treatment. With OCT, light waves are used to capture detailed images of the retina. With FA, a special dye is injected into your bloodstream through an IV. This highlights the blood vessels in the retina so we can determine if there is any bleeding, leakage, or damage
Treatment and Prognosis
Prevention is the best treatment for diabetic retinopathy. Optimal blood sugar, blood pressure, cholesterol and weight control can reduce the long-term risk of vision loss from diabetic retinopathy. Cooperation with your primary care physician is very important to help keep your diabetes and other cardiovascular risk factors under control
Once the diagnosis of diabetic retinopathy has been made, you may require more frequent eye exams. In addition, checking your blood sugar at home, recording your blood sugars in a notebook, and showing these numbers to your primary care physician are critical to success in controlling your disease
Medical Treatment
Medical treatment for diabetic retinopathy may involve the use of injections of medicine into your eye (intravitreal injections) to treat the build up of fluid (diabetic macular edema). Recent science has shown that DME and PDR are controlled by a signal sent from the damaged retina called vascular endothelial growth factor (VEGF). Several VEGF blocking drugs (including Lucentis, Avastin and Eylea) and other medications (steroids and steroid implants) when injected into the eye can cause DME and PDR to regress. Most of these agents provide only temporary relief and need to be given repeatedly over a prolonged period of time.
Laser Treatment
Laser treatment may be recommended for people with diabetic macular edema (DME). The goal of this treatment is to prevent further vision loss. The laser seals leaking blood vessels, reduces swelling and prevents new abnormal blood vessels from growing. For macular edema, the laser is focused on parts of the retina outside of the macula. Multiple laser treatments may be necessary. Laser treatment is not a curative procedure and does not always prevent further loss of vision.
Surgical Treatments
Vitrectomy surgery in the operating room may be recommended if bleeding from diabetic retinopathy causes a vitreous hemorrhage and associated vision loss. Additionally, surgery may be needed to treat tractional retinal detachment in the setting of extensive blood vessel and scar tissue growth.
Vitrectomy surgery requires a team approach. Before surgery, you will likely need to have a physical examination with your general doctor to identify and possibly treat any medical conditions. Your surgeon and anesthesiology team will decide whether local or general anesthesia is appropriate for you. Most vitrectomy surgeries are performed as outpatient procedures with local anesthesia, and the patient may go home the same day. The length of the operation varies from 20 minutes to several hours depending on your condition. Other procedures may be combined with your vitrectomy, including peeling membranes or laser application, depending on your specific needs. Your surgeon will perform your vitrectomy using a microscope and tiny instruments that are placed into your eye through small incisions in the sclera, the white part of your eye.
If you have any questions or concerns about diabetic retinopathy treatment, please discuss them with your Retina Consultants of Texas physician.
What is Age-Related Macular Degeneration?
Age-related macular degeneration (ARMD or AMD) is the most common cause of irreversible vision loss in the United States, affecting up to 20 percent of people over the age of 60. It is one of the most common conditions that our board-certified retina specialists treat on a daily basis.
AMD is caused by the deterioration of the macula, which is the central area of the retina. This condition causes a loss of central vision that occurs slowly over time. At Retina Consultants of Texas, we work in partnership with each patient to create a customized treatment plan to help slow or stop the progression of the disease.
Types and Symptoms of AMD
AMD usually appears after age 50, and the disease is often bilateral (occurring in both eyes). In addition, patients generally have a significant family history of the disease. Patients with AMD may notice a worsening of their central vision while retaining good peripheral vision. Symptoms of AMD can include:
- Visual distortion, including warping or bending of straight lines and objects
- Blurred central vision in one or both eyes
- Difficulty with reading or close-up work
- Increasing difficulty adapting to changing light conditions, especially low light levels
There are two kinds of age-related macular degeneration (AMD): dry and wet. Both forms can lead to vision loss, and patients can have either or both.
Dry AMD
More than 90% of patients diagnosed with AMD have the dry form, which is often associated with a slower progression of the disease that occurs over many years. It is characterized by drusen formation (yellow deposits under the retina that are made up of lipids, a fatty protein), retinal degeneration, and a gradual wearing away of the retina called atrophy. If these areas of retinal degeneration group together into larger areas, it is called geographic atrophy which is a more advanced stage of the disease. Most patients with early dry AMD with mild retinal changes will have no or minimal problems with their vision. However, in its most advanced form, dry AMD can cause profound central vision loss, often with preserved peripheral (side) vision.
Wet AMD
This form of AMD is characterized by the development of abnormal blood vessels known as choroidal neovascular membranes (CNVM) that disrupt the retina and cause leakage of fluid. This growth of abnormal blood vessels can result in vision loss due to fluid build-up in the retina (macular edema), bleeding in the retina, and scar tissue formation (fibrosis). Wet AMD is generally associated with more rapid visual loss over days to weeks compared to the slower progression of dry AMD.
Known Causes
Age-related macular degeneration (AMD) usually occurs after age 50 and is often bilateral (present in both eyes). While the exact cause is unknown, genetics play a role. Many patients have a significant family history of AMD. In addition, numerous studies have revealed that nutritional and lifestyle factors play a role in both the onset and progression of macular degeneration, including:
- Obesity
- Poor diet (especially high levels of saturated fat)
- High blood pressure and cholesterol levels
- Smoking cigarettes
- Cardiovascular disease
Diagnosis
Regular eye examinations are important to diagnose and manage AMD. While being evaluated by your eye doctor, you may undergo multiple types of ocular imaging, including photography, ocular coherence tomography (OCT), and fluorescein angiography (FA) to help with your diagnosis and specific treatment plan.
Ocular coherence tomography (OCT)
This is a non-invasive ophthalmology imaging method that uses light to capture high-resolution, 3D images of the back of the eye. It allows your retina specialist to see the back of the retina and understand what is taking place.
Fluorescein angiography (FA)
This is an imaging study of the blood supply to the retina. Fluorescein dye is injected into the vein of an arm, and this yellow dye passes through the blood vessels in your retina. A specialized camera is then used to take digital photographs of the blood vessels.
Because age-related macular degeneration can be hereditary, adult relatives of AMD patients should see a retina specialist for a baseline evaluation and dilated eye exam.
Treatment and Prognosis
There is currently no cure for either dry or wet AMD. However, there are a number of things you can do to slow the progression of the disease.
Smoking is toxic to the retina and can contribute to AMD progression. If you smoke, stop smoking as soon as possible! Other ways to optimize your retinal health include eating a healthy diet with regular vegetables and fruits, and maintaining a healthy body weight.
The risk of vision loss from some forms of AMD can be reduced by taking a special combination of supplements. The Age-Related Eye Diseases Studies (AREDS & AREDS2), which were large clinical trials, demonstrated a decreased risk of visual loss from moderate dry AMD by taking a combination of the following:
- 15 mg of Beta-carotene
- 400IU of Vitamin E
- 500 mg of Vitamin C
- 80 mg of Zinc
- 2 mg of copper
- Lutein/Zeaxanthin
In addition, an Amsler grid is a chart to use at home to help monitor your vision. Use it daily for each eye as directed and if you notice changes in your vision, contact your ophthalmologist as soon as possible.
Incredible advances in our ability to treat wet AMD since the early 2000s have revolutionized patient outcomes. Before that time, a diagnosis of wet AMD carried a very poor prognosis with most eyes progressing to severe vision loss. Fortunately, medications now available can benefit over 90% of wet AMD patients. These medications primarily target VEGF (vascular endothelial growth factor), a molecule responsible for the abnormal blood vessels which cause damage in wet AMD.
Repeated injections of anti-VEGF agents (Avastin, Lucentis & Eylea) have been firmly established as the optimal treatment for wet AMD. These powerful drugs are given as injections into the eye to suppress abnormal blood vessel growth and leakage. Because these injections are not a cure, but only a treatment, they have to be administered repeatedly (sometimes as often as monthly, indefinitely) in order to have their maximal vision-improving results. Extensive numbing of the eye makes this injection procedure virtually painless.
If you have AMD, you should:
- Stop smoking.
- See your retina specialist regularly.
- Consider AREDS supplements.
- Check your Amsler grid daily.
- Eat a healthy diet with plenty of vegetables and fish.
- Maintain a healthy body weight
About Retinal Tears
As the vitreous gel in the back of the eye starts to liquefy, it can separate from the retina, a condition called posterior vitreous detachment (PVD). If the vitreous gel adheres too firmly to the retina, a retinal tear can occur with a PVD. The tear can also progress to a retinal detachment, a more serious condition that happens when fluid leaks through the tear and separates the retina from the back of the eye.
Causes and Symptoms
Light passes to your retina through a large space in the center of the eye called the vitreous cavity. This cavity is filled with a clear, jelly-like substance called vitreous which is normally in contact with the retina. A posterior vitreous detachment (PVD) occurs when the vitreous gel separates from the retina. This happens in most eyes as we age and tends to occur earlier in myopic (nearsighted) eyes and after trauma or eye surgery. In most cases, this separation does not cause any significant problems. However, when a posterior vitreous detachment occurs, the vitreous gel sometimes pulls holes or rips tears in the retina.
Symptoms of a retinal tear can include the sudden appearance of floaters (black spots) or flashes of light. However, some patients experience very few symptoms. If a vitreous hemorrhage (bleeding) or retinal detachment also occurs, additional symptoms can include blurred vision or loss of peripheral (side) vision.
Diagnosis
A retinal tear can be diagnosed through a thorough dilated eye exam. Sometimes our physicians order an ophthalmic ultrasound to assist with the diagnosis.
Treatment and Prognosis
The prognosis is good if a retinal tear is caught early before it progresses to a retinal detachment. Treatment can include:
- Laser Treatment: The laser causes scarring to the underlying tissue so the retinal tear can be sealed. This prevents fluid from getting under the retina. This procedure is performed in our office.
- Cryotherapy: Cryotherapy offers a similar result by freezing the area to seal the tear, preventing further damage. It is also performed in our office.
Both of these methods are used to prevent the retinal tear from developing into a retinal detachment. Surgery may be necessary if a retinal detachment has already developed along with the retinal tear.
Our sub-specialized, board-certified ophthalmologists at Retinal Consultants of Texas are experienced in treating both retinal tears and retinal detachment.
While retinal tears generally do not cause long-term vision loss and can be effectively repaired through minimally invasive techniques or laser treatment, it is important that the condition is caught early. If not, a retinal detachment may occur which almost always causes vision loss or blindness. At Retina Consultants of Texas, we will evaluate each case promptly, offering a fast and effective diagnosis so treatment can be performed before further damage occurs.
About RVO
A retinal vein occlusion (RVO) occurs when one of the veins that drains blood from the retina in the back of your eye becomes blocked. A blocked retinal vein damages the retinal blood vessels and can lead to hemorrhage (bleeding), impaired blood flow, and leakage of fluid and blood components (hard exudates) into the retina. RVO can cause visual impairment in four ways:
- Blood and hard exudates can directly interfere with retinal function.
- Abnormal fluid can accumulate in the retina, leading to thickening and the presence of cyst-like fluid collections that distort normal retinal architecture. This is called cystoid macular edema(CME).
- Inadequate blood flow to the retina, which is called ischemia
- Abnormal blood vessels can grow from the surface of the retina. This is called neovascularization. These fragile blood vessels can bleed and form damaging scar tissue. Sometimes, these abnormal blood vessels can grow on the iris and drainage canals in the eye, leading to increased eye pressure (neovascular glaucoma).
Our board-certified ophthalmologists at Retina Consultants of Texas are experienced and trained in the diagnosis and treatment of retinal vein occlusions.
There are two different types of retinal vein occlusion (RVO):
- Central Retinal Vein Occlusion (CRVO): Central retinal vein occlusion (CRVO) occurs when the main vein that drains the retina becomes blocked.
- Branch Retinal Vein Occlusion (BRVO): Branch retinal vein occlusion (BRVO) occurs when one of the smaller retinal veins becomes blocked.
Causes and Symptoms
Diabetes, high blood pressure, poorly controlled cholesterol and smoking can all increase a patient’s risk of RVO. Many other conditions can cause RVO, including glaucoma, inflammation and blood clotting disorders (hypercoaguable states). Depending on your clinical situation, you may need to be evaluated for these less common conditions.
The most common symptoms of RVO include:
- Blurred and distorted central vision
- Dim vision
- Decreased sensitivity to light
Sometimes, however, patients with CRVO or BRVO experience no symptoms.
Diagnosis
Your Retina Consultants of Texas physician may obtain multiple types of ocular imaging, including photography, ocular coherence tomography (OCT) and fluorescein angiography to help with your diagnosis and treatment.
Treatment and Prognosis
Depending on the cause and severity of a BRVO or CRVO, treatment may include one or more the following:
- Close clinical observation
- Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) medications (Lucentis, Avastin, Eylea) or steroids
- Laser therapy
- Vitrectomy surgery
In addition to treatment of your eye, if you have CRVO or BRVO, it is very important that you work with your primary care physician to optimally control your cardiovascular risk factors, including blood pressure, cholesterol, weight and diabetes.
Treat RVO Today
The board-certified retinal specialists at Retinal Consultants of Texas work with each patient to diagnose and treat retinal vein occlusion. If found early, RVO can be treated so that further blockage of the veins to the retina do not progress and cause further damage. Our Southeast Texas retina practices offer numerous locations, each equipped to accurately and effectively diagnose, treat, and help manage RVO. Please call one of our area centers to schedule your appointment.